What is Shoulder Arthroscopy?

Shoulder arthroscopy is a minimally invasive procedure used to diagnose and treat various conditions affecting the shoulder joint. It is a modern technique that allows for direct visualization inside the joint, enabling accurate identification and immediate repair of shoulder damage, typically without requiring hospitalization.
The shoulder is a joint capable of movement across multiple planes, making it particularly vulnerable to injuries. In the past, the only treatment option was open surgery, which involved extensive trauma to the joint, prolonged hospital stays, and immobilization with pain lasting for weeks. The groundbreaking arthroscopic method has resolved many of these issues.
Orthopedic Surgeon – Sports Medicine Specialist Dr. Anastasios Deligeorgis is highly trained in the latest arthroscopic surgical techniques, having completed his training in internationally accredited orthopedic centers. He has served as a Clinical Instructor in arthroscopy at major international hospitals and conferences. Additionally, the 3rd Orthopedic Clinic of Hygeia Hospital, where he is the Deputy Director, is one of the few orthopedic centers in Greece internationally certified as an arthroscopic surgery training center.
Shoulder Anatomy
The shoulder is a complex joint with the greatest range of motion of any joint in the human body. It connects the upper part of the humerus (arm bone) with the scapula (shoulder blade) and the distal end of the clavicle (collarbone).
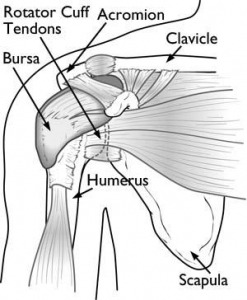
Humeral Head: The upper part of the humerus forms a spherical head that fits into the glenoid cavity of the scapula. Both surfaces are covered with articular cartilage, which provides smooth movement and absorbs shocks during activity.
Labrum: The rim of the glenoid cavity is lined with a strong fibrocartilaginous tissue called the labrum, which deepens the cavity and helps stabilize the joint.
Joint Capsule: The shoulder joint is surrounded by a capsule that produces synovial fluid for lubrication. Various ligaments also surround and stabilize the joint.
Rotator Cuff: Four tendons form the rotator cuff, keeping the humeral head centered within the shallow glenoid cavity. These are the tendons of the supraspinatus, infraspinatus, subscapularis, and teres minor muscles.
Subacromial Bursa: Above the rotator cuff and beneath the acromion (the bony part of the scapula above the humeral head) lies the subacromial bursa. This fluid-filled sac allows the rotator cuff to glide smoothly during arm elevation.
Description of Shoulder Arthroscopy
The orthopedic surgeon inserts an arthroscope—a tiny camera with strong lighting—through a small incision (about 3–5 mm) in the shoulder skin. The internal view of the joint is then magnified and displayed in high resolution on a screen.
This enables the surgeon to:
- Carefully examine the interior of the shoulder joint, identifying even the smallest and hardest-to-reach lesions.
- Repair intra-articular and periarticular damage using specially designed micro-instruments and inert implant materials such as sutures and anchors. Examples include tendon repair for tears, release of adhesions, and labral repairs after dislocations.
The incisions are only a few millimeters wide (unlike the large incisions in open surgery), causing minimal muscle and tissue trauma. This results in fewer complications and significantly less postoperative pain. Any small scars tend to fade over a few months.
In some cases, biological therapies such as Stem Cell or Platelet-Rich Plasma (PRP) injections may be applied alongside arthroscopy to aid healing.
In most cases, shoulder arthroscopy lasts no more than an hour. It is typically performed under a combination of regional and light general anesthesia, depending on the patient’s medical history, and the patient returns home the same day.
Get the Help You Need Today!
New Arthroscopic Techniques
ΗArthroscopic surgery has seen rapid development in recent years, constantly evolving with new techniques and specialized tools that make it increasingly less invasive. Different advanced arthroscopic techniques are applied depending on the type and severity of the injury.
In simple injuries, immediate repair is performed (such as tendon suturing or adhesion release), while in more severe cases, more complex and advanced techniques can be applied according to international literature. Indicatively:
- In massive, irreparable rotator cuff tears, reconstruction of the superior capsule may be performed using a graft from the patient (autograft), or tendon transfers may be done to substitute the function of a specific muscle.
- In recurrent dislocations and cases with significant bone loss in the shoulder joint, an autologous bone graft (bone block technique) from the iliac crest may be used, or the coracoid process may be transferred (Latarjet technique).
- In rotator cuff tears, especially chronic ones, additional reinforcement of the repair is often required—not only mechanically but also biologically. This can be achieved using stem cells, platelet-rich plasma (PRP), cells from the subacromial bursa, or autologous tendon grafts such as the long head of the biceps tendon. The aim is to enhance healing of the repair and improve the clinical outcome.
Advancements in arthroscopy not only concern techniques but also materials. New “low-profile,” high-tech, durable, and biocompatible materials are increasingly being used. For example, “all-suture anchors” are now commonly used—much smaller than conventional anchors, very strong, and composed solely of sutures instead of metal or other hard materials.
With these smaller anchors, more can be placed in the same tear area, thus providing stronger repair. They also allow for postoperative MRI imaging, if needed, to evaluate the repair and tendon integrity—something that was not possible in the past with metal anchors. Lastly, in case of a re-tear, revision surgery is much easier since there are no large metal components present.
Advantages of Shoulder Arthroscopy
Arthroscopic surgery offers several advantages compared to open surgery:
- Minimally invasive method
- Minimally traumatic (very small incisions)
- High diagnostic accuracy (detailed imaging of the joint interior)
- No hospitalization required
- Significantly lower risk of complications
- Minimal postoperative pain
- Immediate mobilization
- No postoperative scarring
- Quick return to daily activities
- More effective and faster recovery
Indications for Shoulder Arthroscopy
Shoulder arthroscopy is primarily performed for the treatment of the following conditions:
- Rotator cuff tears
- Labrum and shoulder ligament tears from dislocations or acute/chronic instability
- Persistent calcific tendinitis
- Shoulder stiffness (Frozen Shoulder)
- Conditions affecting the long head of the biceps tendon
- Articular cartilage injuries or lesions
- Suprascapular nerve entrapment
- Impingement syndrome
- Synovial membrane diseases
- Presence of loose intra-articular bodies
- Selected fractures
- Early-stage arthritis
Get the Help You Need Today!
Postoperative Recovery
After surgery, the use of a special shoulder sling is usually recommended for the first few days, which allows basic daily hand use. Postoperatively, pain is typically minimal, and mild painkillers are prescribed preventively for the first few days.
The patient must be regularly monitored by the doctor to assess wound healing progress and receive guidance for mobilization. If stitches are present, they are typically removed after 8–10 days.
A successful postoperative outcome requires the patient to follow a specific rehabilitation program.
Physiotherapy
Physiotherapy is essential for patient recovery, mainly through exercises that the patient can perform at home under the guidance of a physiotherapist or doctor. The physiotherapy program is personalized based on the type and extent of the injury that was treated arthroscopically.
Συχνές ερωτήσεις για την αρθροσκόπηση ώμου
Unlike other procedures, shoulder arthroscopy is a minimally invasive procedure. Therefore, in most cases, the patient can return home just a few hours after the operation.
First, it should be emphasized that each patient’s case is different. The type of anesthesia administered depends on the patient’s medical history as well as the severity of their condition. However, in most cases, shoulder arthroscopy is performed under a combination of local anesthesia and mild general anesthesia.
Complications after shoulder arthroscopy are rare. Theoretically, every surgery carries some risk of complications, such as infection at the surgical site, swelling, or nerve damage. However, the likelihood of these occurring during shoulder arthroscopy, which is a minimally invasive surgery, is extremely low. Furthermore, systematic post-operative monitoring significantly reduces the chance of complications.
Key factors that influence the likelihood of complications include the surgeon’s skill and experience, the size of the surgical trauma, consistent post-operative monitoring, and the patient’s adherence to the prescribed physiotherapy program.
Each patient’s situation is unique. Therefore, it is not possible to define a fixed cost for the procedure. The cost depends on the extent of the damage, the specific materials used, and the type of medical equipment required (specialized or not), among other factors.
If, after reading the detailed information about shoulder arthroscopy, you recognize similar symptoms in yourself, please contact the physician. Together, you can find the most appropriate and personalized solution for your case.