What are sports injuries?

The term “sports injuries” refers to any injury that occurs during athletic activity, whether at a professional or amateur level.
Sports injuries are divided into acute injuries and overuse injuries. They most commonly affect muscles, tendons, bones, ligaments, and articular cartilage.
What causes sports injuries?
Accidents, poor training techniques, inappropriate sports equipment, inadequate warm-up, or overtraining are some of the main factors that can lead to injury.
How are sports injuries different?
Sports injuries are not exclusive to athletes, but they occur more frequently among those involved in sports. Athletes represent a unique category of individuals. Even a minor injury that causes a missed training session or prevents peak performance is significant. For professional athletes, an injury could cost them a medal, a season, a contract, or even their entire career. For amateur athletes, it might mean stepping away from their favorite activity, which can affect their mood and mental balance.
In this context, Sports Medicine has advanced diagnostic and treatment methods for sports injuries. However, these methods are not only for athletes but are applied to anyone suffering from such injuries.
What are the most common sports injuries?
- Muscle injuries
- Ligament injuries / Sprains / Ligament ruptures
- Meniscus tears
- Tendonitis / Tendinopathy / Tendon ruptures
- Articular cartilage tears
- Stress fractures
- Iliotibial band syndrome
- Periostitis
- Plantar fasciitis
Get the Help You Need Today!
What is the proper treatment for sports injuries?
ΗAdvancements in medical science have led to effective and modern treatments, helping athletes return to their sport as quickly as possible with minimal complications and reduced risk of recurrence.
A major contribution has come from new biological therapies, including:
- Autologous growth factors from the patient’s own blood – Platelet-Rich Plasma (PRP)
- Stem cell therapies
These treatments do not involve drugs or foreign substances and are fully compatible with the body and in compliance with World Anti-Doping Agency (WADA) regulations.
Additionally, modern arthroscopic surgeries and minimally invasive techniques play a crucial role in the specialized treatment and rapid return to physical activity.
Muscle Injuries
What are they?
Muscle injuries, commonly known as strains, can result from direct impact or indirect force when the muscle is overstretched beyond its capacity.
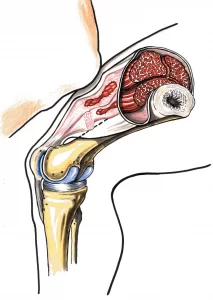

Depending on severity, they are classified into three grades:
- Grade I: Mild strain, with overstretching or minor fiber tears
- Grade II: Partial muscle tear
- Grade III: Complete muscle rupture
What are the main causes of muscle injuries?
Strains most commonly occur in muscles that cross two joints, such as:
- Hamstrings
- Rectus femoris (part of the quadriceps)
- Gastrocnemius
- Biceps brachii
Predisposing factors include:
- Previous muscle strain
- Muscle imbalance
- Muscle fatigue
- Inadequate rest
- Muscle weakness
- Inadequate warm-up
- Improper equipment (e.g., footwear)
How is diagnosis made?
Diagnosis is usually based on patient history and clinical examination.
For Grade II and III injuries, ultrasound or MRI can confirm the diagnosis.
An X-ray may be used to rule out an avulsion fracture where the tendon attaches to the bone.
What is the proper treatment?
Initial treatment typically includes:
- Rest
- Ice therapy
- Compression bandaging
- Leg elevation
These help minimize symptoms, hematoma, and inflammation.
Physical therapy may be introduced in the early stages, followed by a rehabilitation program with stretching, strengthening exercises, and sport-specific training to help the athlete return to their prior level of activity.
It is also essential to identify and correct predisposing factors that led to the injury.
New biological techniques like PRP are especially useful in chronic cases, particularly when the injury involves the muscle-tendon junction or the tendon itself.
Get the Help You Need Today!
Ligament Injuries
Anatomy
Ligaments are thick bands of connective tissue made up of collagen fibers that connect bones to each other at the joints. Their main function is to stabilize the joints, but they also play a significant role in proprioception — the body’s ability to sense its position and movement in space.
Mechanism of Injury
Ligament injuries typically occur due to a sudden overload, where the ligament is stretched as the joint is forced into an extreme position — commonly referred to as a sprain.
Ligament injuries are classified by severity into:
- Grade I: Simple stretching
- Grade II: Partial tear
- Grade III: Complete tear
Common Locations for Ligament Injuries
Knee:
- Injury or tear of the Anterior Cruciate Ligament (ACL)
- Injury or tear of the Posterior Cruciate Ligament (PCL)
- Injury or tear of a Collateral Ligament
- Combination of injuries or tears involving more than one ligament
Ankle (Ankle Sprains):
- Involvement of the Medial (Deltoid) Ligament
- Lateral Ligament
- Anterior Tibiofibular Ligament
- Syndesmosis (tibiofibular joint)
- Combinations of the above
Symptoms
The main symptoms are pain and swelling, usually proportional to the extent of the ligament damage. There may also be difficulty walking. In cases of complete ligament tear, joint instability may be present, typically noticeable after the acute symptoms subside.
Diagnosis
Diagnosis is based on the patient’s history and clinical examination. The injured area is usually tender and swollen. X-rays help rule out bone fractures.
In suspected cases of severe ligament injury, cartilage damage, or other intra-articular lesions, an MRI scan may be recommended — usually after the acute phase — to provide a clear diagnosis. Complete ligament ruptures can lead to joint instability and may result in more severe cartilage damage if left untreated.
Treatment
Conservative Management
In the early hours and days following injury, the focus is on symptom relief and swelling reduction:
- Ice therapy 3–4 times per day for 15–20 minutes
- Elevation of the limb
- Compression with an elastic bandage
- Rest depending on symptoms. In cases of severe pain or walking difficulty, partial weight-bearing with crutches may be necessary.
- Recovery time depends on the injury’s severity, often 3–6 weeks for symptom resolution.
Grade II and III ligament injuries may require more strict immobilization to allow healing.
Biological Therapies
Modern biological treatments like Platelet-Rich Plasma (PRP) or stem cells, either alone or combined with surgery, may enhance healing and reduce recurrence, allowing faster return to sports or activities.
Surgical Management
Depending on the injury’s severity, affected joint, specific ligament involved, and the level of resulting instability, surgery may be necessary — especially when conservative treatment fails, leading to chronic instability, or in cases involving intra-articular damage. Minimally invasive techniques are preferred.
Surgical treatment may include:
- Arthroscopy of the joint to assess and treat intra-articular lesions
- Repair or reconstruction of the torn ligaments
Rehabilitation
Physiotherapy and early mobilization are key to reducing symptoms in the initial stages and gradually restoring function. Specific balance, proprioception, and strengthening exercises help prevent recurrence. Full recovery time depends on injury severity and can take several months.
Get the Help You Need Today!
Tendon Injuries
Anatomy
Tendons are made of connective tissue and connect muscles to bones. Their main function is to transfer muscle power to the skeleton, aiding both movement and joint stability.
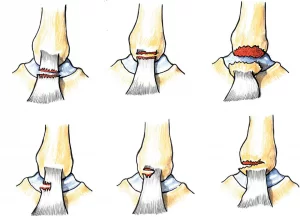
Tendinitis – Tendinopathy. What is it?
Inflammation of a tissue is the body’s natural process to heal it after an injury. It is usually accompanied by swelling, redness, warmth, and pain. When the inflammation involves a tendon, it is referred to as tendinitis.
Tendinopathy typically refers to chronic conditions, often caused by overuse, where there is pain in the tendon but without the signs of acute inflammation. In such cases, the tendon shows degenerative changes, including disorganized collagen fibers and a reduced number of cells. There may also be increased blood vessel formation (neovascularization), and in some cases, localized necrosis with or without calcifications within the tendon.
How Is It Caused?
Tendinitis and tendinopathy are usually the result of repeated microtraumas. A sudden increase in physical activity or inflexible muscles can increase the risk of developing these conditions.
Depending on the sport, athletes are more likely to develop tendinitis in the body area that undergoes the most strain. For example, tennis, volleyball players, and swimmers are more prone to shoulder and elbow tendinitis, while football players, runners, and dancers are more vulnerable in the lower limbs.
Symptoms
Common symptoms include pain during use of the affected limb, which worsens with activity, and swelling around the tendon.
Diagnosis
Diagnosis is based on medical history and physical examination. In chronic cases, the tendon may appear thickened and be tender to palpation and with resisted movements. The range of motion of the adjacent joint may be limited.
Imaging with MRI or ultrasound can confirm the diagnosis and rule out tendon rupture. Plain X-rays may reveal bone changes or intratendinous calcifications.
Treatment
The standard treatment in the acute phase includes:
- Ice therapy
- Rest
- Compression
- Elevation
In the second phase, treatment focuses on:
- Muscle strengthening
- Stretching exercises
- Correction of technical errors and muscular imbalances
Biological Therapies
In chronic cases where inflammation persists or in tendinopathy with tendon degeneration, injecting healing factors from the patient’s own blood—Platelet-Rich Plasma (PRP)—or Stem Cell Therapy may help.
The patient should then follow a specialized rehabilitation and strengthening program.
In rare cases where conservative treatment fails, minimally invasive surgical techniques may be applied.
Tendon Rupture – Partial / Complete: What Is It?
A tendon rupture occurs when the continuity of the tendon is disrupted, making it impossible to transmit force from the muscle to the bone. This results in loss of stability or movement in a joint.
When Does It Occur?
Tendon rupture may be:
- Acute/traumatic: due to a sudden injury, often occurring when the force applied exceeds the tendon’s strength. A typical scenario is during eccentric contraction of a muscle, such as in the calf (gastrocnemius) when a runner pushes off at the start of a sprint.
- Degenerative/overuse-related: resulting from long-term wear and tear.
Rupture may be partial or complete, and can occur:
- At the musculotendinous junction
- In the mid-portion of the tendon
- At the tendon’s insertion into the bone
Acute ruptures are more commonly seen in recreational athletes aged 30–50 who engage in explosive sports, often without prior symptoms.
Risk Factors
Predisposing factors for tendon degeneration and rupture include:
- Chronic tendinitis or tendinopathy
- Sports involving repetitive motions
- Previous injury
- Cortisone injections (especially intratendinous)
- Use of certain antibiotics (e.g. fluoroquinolones)
- Long-term steroid use
- Chronic kidney disease
- Rheumatoid arthritis
- Diabetes mellitus
- Certain autoimmune diseases
Symptoms
In acute ruptures, one may feel a sudden snapping sensation. This is usually followed by swelling and pain in the area. Depending on the tendon affected, there may also be:
- Bruising
- Inability to move the joint or limb
- Difficulty walking if it involves the lower limbs
- A palpable gap at the rupture site
Diagnosis
Diagnosis is based on the patient’s history and clinical examination. MRI or ultrasound confirms the rupture and identifies the exact location and severity.
Treatment
Treatment depends on:
- The affected body area
- The size of the rupture
- The degree of functional impairment
- The patient’s age
- Activity level
- Whether the rupture is recent or chronic
Conservative Treatment
Small or partial-thickness tears may respond well to conservative treatment.
Conservative treatment includes:
- Immobilization of the affected limb, which may last 3–6 weeks depending on the location of the injury
- A rehabilitation program with range of motion exercises, muscle strengthening, and proprioception training
- Biological therapies involving the injection of healing agents, such as Platelet-Rich Plasma (PRP) and stem cell therapy
Surgical Treatment
In most cases, surgical repair is the recommended course of treatment.
The surgical approach depends on the specific area of the body and is typically performed using minimally invasive or arthroscopic techniques. Treatment involves suturing the torn ends of the tendon or reattaching it to the bone using specialized biocompatible materials.
Surgical repair is always followed by a specialized rehabilitation program.
Get the Help You Need Today!
Cartilage Injuries
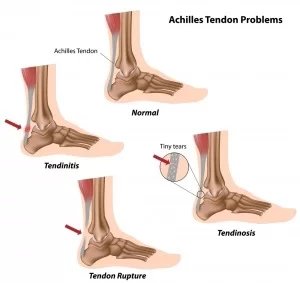
Anatomy
Articular cartilage is the smooth, white, soft tissue that covers the joint surfaces of bones, allowing them to glide smoothly, contributing to seamless motion and absorbing shock. This type of cartilage is known as hyaline cartilage.
What is it?
Articular cartilage can become damaged due to trauma or natural wear and tear. Cartilage injuries often result from sports-related injuries, causing compression or detachment of a portion of the cartilage. The knee joint is most frequently affected, but other joints such as the ankle, hip, shoulder, elbow, and others may also be involved.

Symptoms
When cartilage is damaged, joint function is impaired. This may lead to pain, joint effusion (increased reactive fluid), mechanical symptoms such as locking or clicking due to a loose body, and may ultimately result in early-onset arthritis, i.e., complete joint degeneration.
Diagnosis
Diagnosis is made based on the injury history, symptoms, clinical examination, and MRI findings.
Treatment
Because articular cartilage lacks blood supply, the body cannot naturally repair cartilage damage with normal hyaline cartilage. For this reason, science has developed a range of techniques to restore the cartilage as much as possible and delay the progression of potential arthritis.
New biological techniques include injections of:
- Stem cells or autologous chondrocytes
- Platelet-Rich Plasma (PRP)
Arthroscopic techniques such as:
- Microfractures
- Autologous chondrocyte transplantation
- Transplantation of autologous osteochondral plugs from non-weight-bearing areas
These are some of the treatments we use today, depending on the size and location of the damage, to achieve optimal repair.
Rehabilitation
A proper rehabilitation program involving physiotherapy, strengthening and proprioception exercises, and kinesitherapy is essential to help the athlete return to previous activity levels.
Βρείτε λύση στο πρόβλημα σας!
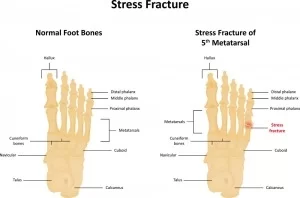
Stress Fractures
What is it?
A stress fracture refers to a small crack or bone edema in a bone, usually caused by overuse and repetitive activity.
It occurs when muscles become so fatigued that they can no longer absorb additional shock. Eventually, the overloaded stress is transferred to the bone, causing a small crack — known as a stress fracture.
What causes it?
Stress fractures are often the result of a sudden increase in the intensity, duration, or frequency of an activity. This is common in young athletes starting a new sport, and also in experienced athletes who, after a period of rest between competitive seasons, resume training at the same intensity/duration without gradual progression. The risk of stress fractures also increases when athletes fail to allow enough recovery time or ignore warning signs of discomfort or pain.
Several other factors — such as training technique and nutrition — may increase the likelihood of developing a stress fracture.
Examples include:
Incorrect Technique
Anything that alters the mechanics by which the foot absorbs impact forces during ground contact increases the likelihood of a stress fracture. Therefore, conditions such as tendinitis, calluses, blisters, or wounds can affect the way forces are distributed during walking or athletic activity, leading to overloading of a bone.
Inappropriate Equipment
Using worn-out shoes or footwear that is unsuitable for a specific sport or individual (depending on the way pressure is distributed) can result in a stress fracture.
Surface Change
A recent change in training surface—such as a tennis player switching from grass to clay courts, or a runner transitioning from treadmill to asphalt—can lead to a stress fracture if the change is not gradual.
Bone Insufficiency
Stress fractures can also occur in individuals with reduced bone density, as in osteoporosis or due to long-term use of certain medications, even during normal daily activities.
Are stress fractures more common in women than in men?
Medical studies have shown that female athletes are more prone to stress fractures. This may be due to a condition known as the Female Athlete Triad, which includes:
- Disordered eating (bulimia or anorexia)
- Amenorrhea (absence of menstruation)
- Osteoporosis
However, eating disorders are not exclusive to female athletes, as an increasing number of male athletes also experience similar issues.
Where and when do they occur?
Most stress fractures occur in the lower limbs. The tibia is the most commonly affected bone, followed by the fibula, tarsal bones, metatarsals, femur, and the pubic ramus of the pelvis. Practically, any bone subjected to repeated, continuous loading can be affected.
Studies show that most stress fractures occur in track and field athletes, tennis players, and gymnasts—sports that involve repetitive loading of the lower limbs. Inadequate rest between training sessions or competitions increases the risk of such injuries.
What are the symptoms and how is it diagnosed?
The most common symptom is pain during activity that progressively worsens and usually improves with rest. Localized tenderness, swelling, or bruising may also be present. It’s crucial for the orthopedic specialist to obtain a detailed medical and activity history and consider all risk factors.
X-rays are often negative in the early weeks, so diagnosis may require a CT scan, bone scintigraphy, or MRI.

Management
First Aid
If an athlete suspects a stress fracture, they should consult a specialized orthopedic doctor. Ignoring the condition may result in serious consequences: a bone crack or bone edema can develop into a complete fracture.
Until the athlete is examined by an orthopedic specialist, the following is recommended:
- Rest
- Ice therapy
- Compression
- Elevation of the limb
Treatment
The goal of treatment is pain relief and bone healing, which typically takes 6–8 weeks.
Treatment depends on the location and severity of the fracture. Most stress fractures are managed conservatively.
The most important factor in treatment is rest. The athlete must stop activities that caused the injury.
In most cases, the athlete can engage in alternative physical activities that do not stress the affected limb, in order to maintain fitness until the fracture heals.
In some cases, walking aids (e.g., crutches), special braces, orthoses, or even casts may be necessary.
Surgery with internal fixation is rarely required.
It is essential that the athlete-patient follows their orthopedic doctor’s rehabilitation plan to return safely and as quickly as possible to their sport. If the athlete resumes activity too soon, the fracture may worsen, heal poorly or not at all, leading to serious long-term problems.
Prevention
Prevention is the most important factor.
Some tips:
- When starting a new sport, increase training volume and intensity gradually.
- Proper warm-up.
- Alternate between sports or training methods to maintain fitness.
- Ensure proper nutrition with adequate calcium and vitamin D intake.
- Use appropriate equipment and footwear.
- In case of pain or swelling, rest for a few days.
- Seek early advice from a specialized orthopedic doctor if pain persists.