What is hip arthritis?
Hip arthritis is a common condition that affects a large percentage of the population over the age of 50, but can also affect younger individuals, although more rarely.
It is a common cause of pain and stiffness in the hip joint. It can cause problems even in simple daily activities such as getting up from a chair or bed, walking, or putting on socks or shoes.
Since arthritis tends to worsen over time, it is best to start managing it early to reduce its impact on quality of life.
What is the anatomy of the hip?
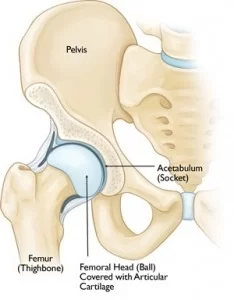
The hip is one of the largest joints in the body. It consists of a hollow surface on the pelvis called the acetabulum and a spherical surface, the femoral head.
The articular surfaces of the acetabulum and the femoral head are covered by articular cartilage—a smooth surface that allows for smooth gliding and absorbs shock during movement and weight-bearing.
The hip joint is surrounded by the joint capsule, a thin membrane that produces synovial fluid. This fluid nourishes and lubricates the cartilage, reducing friction and improving movement.
Types of hip arthritis
Hip Osteoarthritis: What is it?
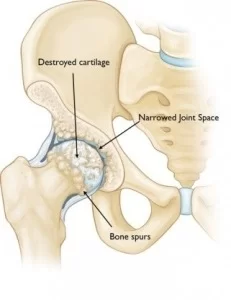
Hip osteoarthritis is a degenerative disease in which the articular cartilage deteriorates and breaks down over time. As the cartilage degenerates, it loses its smooth texture and becomes thinner, leading to friction between the bones and making movement painful. Osteoarthritis progresses slowly, and pain and stiffness worsen over time.
What causes hip osteoarthritis?
Osteoarthritis does not have a single specific cause, but several factors contribute to its development:
- Older age
- Family history
- Previous hip injury
- Obesity
- Congenital hip dysplasia
- Femoroacetabular impingement
It is also possible to develop osteoarthritis even without having any of the above risk factors.
Post-traumatic hip arthritis
Post-traumatic arthritis is hip arthritis that develops after an injury or fracture to the hip.
Rheumatoid arthritis: What is it?
Rheumatoid arthritis is a chronic condition that affects many joints, including the hip. It is an autoimmune disease, meaning the body’s immune system attacks its own tissues, resulting in the destruction of cartilage, ligaments, and bones. The inflammation starts in the membrane that lines the joint (the synovium) but spreads to surrounding tissues, making movement difficult and painful. Inflammation can lead to joint deformity and destruction.
What are the main symptoms of rheumatoid arthritis?
The most common symptom is pain in the hip area. It usually develops gradually and worsens over time, although it can sometimes have a sudden onset.
- Initially, pain and stiffness are usually worse in the morning or after rising from a sitting position.
- Pain progressively worsens with activity and may become constant in advanced stages.
- Pain may be located in the hip or thigh and may radiate to the buttock or knee.
- Pain usually worsens with activity.
- Stiffness can make walking or bending difficult.
- There may be a feeling of tightness or noticeable joint crepitus.
- Many patients also report increased pain with weather changes, especially in humidity.
How is rheumatoid arthritis diagnosed?
The medical history and clinical examination help in diagnosing arthritis. Additional tests, such as standard X-rays, can confirm the diagnosis.
What is checked during the clinical examination for rheumatoid arthritis?
During the clinical exam, your orthopedic specialist will assess:
- Tenderness and pain in the hip area
- Joint crepitus during movement
- Reduced range of motion
- Pain during weight-bearing exercises
- Gait abnormalities
- Muscle strength issues
Get the Help You Need Today!
Imaging tests
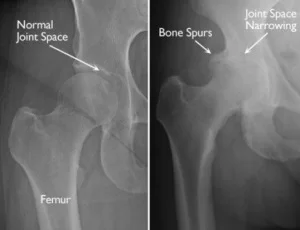
X-rays:Radiographic examination can show narrowing of the joint space, the presence of bony overgrowths (osteophytes), subchondral bone sclerosis, and the presence of subarticular cysts.
Other imaging tests:Less commonly, an MRI or CT scan may be needed.
Rheumatoid arthritis: What is the appropriate treatment?
Conservative treatment
There are several conservative measures one can try in the early stages, especially when quality of life has not been significantly affected.
Lifestyle Changes
Some changes in daily activities can help slow the progression of arthritis and reduce symptoms:
- Avoid activities that exacerbate symptoms, such as climbing stairs.
- Incorporate activities into your routine that strengthen the muscle system supporting the hip while maintaining or improving range of motion. A very good low-impact exercise is swimming.
- Weight loss can help reduce joint load, thus decreasing pain and improving mobility.
Physiotherapy
A specialized program of exercise and movement therapy can increase flexibility and range of motion while also strengthening the core and hip muscles.
Medication
If pain affects your daily life, you may need to take some medication.
- Paracetamol (e.g., Depon, Panadol, or Apotel) is a relatively simple painkiller that can help reduce arthritis pain. You should consult a doctor for the appropriate dosage and regimen.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) can also help reduce inflammation and pain. A doctor’s advice is essential before taking these medications.
Injectable Treatments
Local injections of hyaluronic acid or cortisone can also help relieve symptoms.
Regenerative Medicine
Promising biological therapies like Platelet-Rich Plasma (PRP) or Stem Cells (STEM CELLS) may help reduce symptoms and possibly delay disease progression.
Surgical Treatment
If symptoms do not improve with conservative methods, you may be a candidate for surgery.
Total Hip Replacement: What Is It?
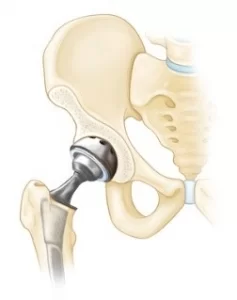
The most common and effective surgical treatment is Total Hip Replacement. The orthopedic surgeon removes the damaged parts of the hip socket and femur and replaces them with biocompatible materials made from special metal alloys and polyethylene (a type of plastic) or ceramic parts.
With modern minimally invasive total hip replacement techniques, tissue damage is significantly reduced, leading to faster and less painful recovery and a quicker return to daily activities.
Get the Help You Need Today!
What Are the Possible Complications of Total Hip Replacement?
- Infection
- Blood loss
- Deep vein thrombosis
- Pulmonary embolism
- Dislocation of the prosthetic joint
- Leg length discrepancy
- Damage to blood vessels or nerves
- Perioperative fracture
What Should You Be Careful About During Recovery?
After any surgery, there is a recovery period. This period varies from person to person and depends on the details of the surgery, the patient’s previous condition, any coexisting medical conditions, and the state of the muscular system.
A good, individualized rehabilitation and physiotherapy program will help the patient return more quickly to daily activities.