Shoulder Dislocation: What is it?
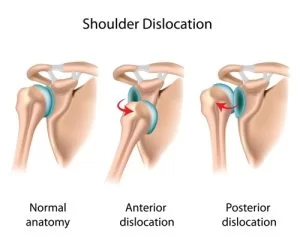
The term shoulder dislocation describes the condition in which the head of the humerus bone moves away from the glenoid cavity, which is its normal position (shoulder dislocation).
The shoulder can either fully come out of the joint or partially come out and then return to its normal position (shoulder subluxation).
The affected person should immediately consult an orthopedic surgeon to have the shoulder relocated (reduced) through special maneuvers if needed, and to diagnose any associated injuries.
Depending on the direction of the humeral head displacement during dislocation, it can be classified as anterior (the most common), posterior, or multidirectional.
When does dislocation lead to shoulder instability?
When the humeral head dislocates, certain anatomical structures of the shoulder are inevitably damaged. If these injuries are not treated promptly and properly after the first episode, recurrence of the dislocation is likely. The problem can become chronic, causing instability of the shoulder joint (a tendency of the shoulder to dislocate), which complicates not only athletic activities but also the patient’s daily life.
Each new dislocation increases the risk of further damage to shoulder tissues such as the cartilage covering the joint surfaces, the labrum cartilage, and even the bones. It may cause a fracture (tear) on the front part of the glenoid (bony Bankart lesion) or an impaction fracture on the humeral head (Hill-Sachs lesion). These fractures can create bone defects that in turn cause greater instability, significantly increasing the chance of recurrent dislocations. In older patients, shoulder dislocation can lead to tendon tears (rotator cuff tears) and weakness in arm use.
Moreover, all these injuries increase the future risk of developing arthritis (joint degeneration).
Shoulder Dislocation: What are the main causes?
Usually, shoulder dislocation results from high-impact trauma, most often during sports activities. However, sometimes it can occur due to mild injuries in patients with loose connective tissue (hypermobility) and increased joint laxity in the shoulder.
What symptoms does shoulder dislocation have?
Common symptoms of shoulder dislocation include:
- Severe pain
- Inability to move the joint
- Deformation of the joint
- Neurological symptoms such as numbness or other sensory disturbances in the shoulder
Additionally, in cases of chronic shoulder instability:
- Pain during certain movements and less frequently at rest or at night when trying to sleep on the affected shoulder
- Constant fear that the shoulder will dislocate when raising the arm above shoulder level
- Recurrences of dislocation, even during sleep
Get the Help You Need Today!
Shoulder Dislocation: How Is the Diagnosis Made?
The diagnosis of shoulder dislocation is made based on:
- The history of the injury
- The patient’s symptoms
- Clinical examination
- X-rays
After the dislocation is reduced, damage assessment is performed using MRI, CT arthrography, or MR arthrography. Simple X-rays help exclude other injuries.
What treatment options are available for shoulder dislocation?
After reduction, the treatment method—conservative or minimally invasive (arthroscopy)—is decided depending on several factors, including:
- The existing injuries
- The presence and size of any bone damage
- The patient’s age at the time of the first dislocation
- The number of dislocations
- The patient’s sports activities
Internationally, it has been observed that the younger the patient at the time of the first dislocation and the higher their activity level, the greater the chance of a second dislocation in the future. For example, a 20-year-old athlete has nearly a 100% chance of a second dislocation regardless of conservative treatment.
What does conservative treatment of shoulder dislocation include?
Conservative treatment includes:
- Avoiding activities that worsen symptoms
- Immobilization of the shoulder in a sling for a few weeks until the pain subsides
- Taking painkillers and non-steroidal anti-inflammatory drugs
- Physical therapy with mobilization exercises and strengthening of the shoulder muscles
Generally, conservative treatment yields good results in older patients, with low activity levels and no associated shoulder injuries.
When conservative treatment is ineffective or for young patients with intense athletic activity or significant anatomical damage, arthroscopic surgery is the treatment of choice.
Arthroscopy – Definitive treatment without hospitalization
Modern arthroscopic techniques provide definitive shoulder stabilization with excellent functional results. Using a tiny camera and special micro-instruments inserted through millimeter-sized incisions (3-8 mm) without opening the joint, a specialized orthopedic surgeon can reposition the injured tissues anatomically and suture any torn tendons. Suturing and repositioning are performed using specially designed implants (anchors) and strong sutures.
In cases of significant bone damage, especially in contact sport athletes, bone grafting procedures are performed using arthroscopic techniques to fill bone defects. Grafts may be autografts taken from the patient’s pelvis or coracoid process (a bone near the shoulder joint, as in the Latarjet procedure), or allografts (grafts from another donor after special processing).
The patient does not require hospitalization and can return home the same day after a few hours.
Rehabilitation
After surgery, the patient can immediately use the arm for activities performed in front of the body. However, to protect the shoulder from sudden movements and allow rest, a brace (sling) is worn to partially immobilize the arm for 3-4 weeks.
This is followed by a specialized rehabilitation and physical therapy program to help the patient return quickly to previous daily and athletic activity levels. Recovery time varies depending on the severity of the injury, patient compliance, and functional demands. Return to simple daily activities and office work (typing, writing) is immediate, while return to full activities takes approximately 2 ½ to 3 ½ months, and return to full athletic activities occurs after about 6 months.